by Ken DeRouchie | May 29, 2007 | Articles, Featured Veterinary, Issue 03, Newsletter, Practice Areas, Veterinary
Lab tests have shown that an injection of a liquid polymer known as polyethylene glycol (PEG), if administered within 72 hours of serious spinal injury, can prevent most dogs from suffering permanent spinal damage. Even when the spine is initially damaged to the point...

by Ken DeRouchie | May 29, 2007 | Articles, Featured Optometry, Issue 03, Newsletter, Optometry, Practice Areas
NEW NIH STUDY LINKS LEAD EXPOSURE WITH INCREASED RISK OF CATARACT Results from a new study show that lifetime lead exposure may increase the risk of developing cataracts. Researchers found that men with high levels of lead in the tibia, the larger of the two leg bones...

by Ken DeRouchie | May 29, 2007 | Articles, Featured Veterinary, Issue 03, Newsletter, Practice Areas, Veterinary
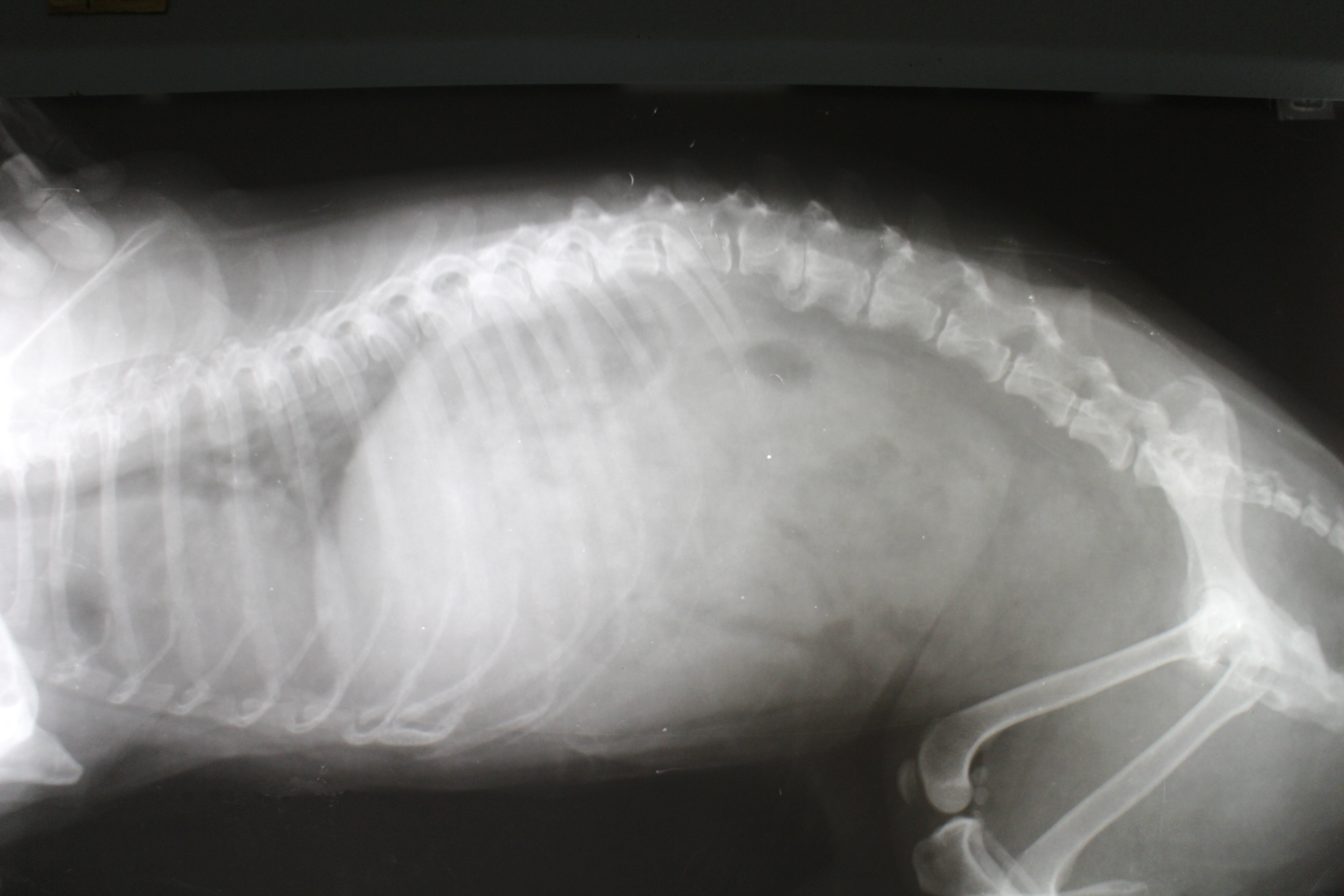
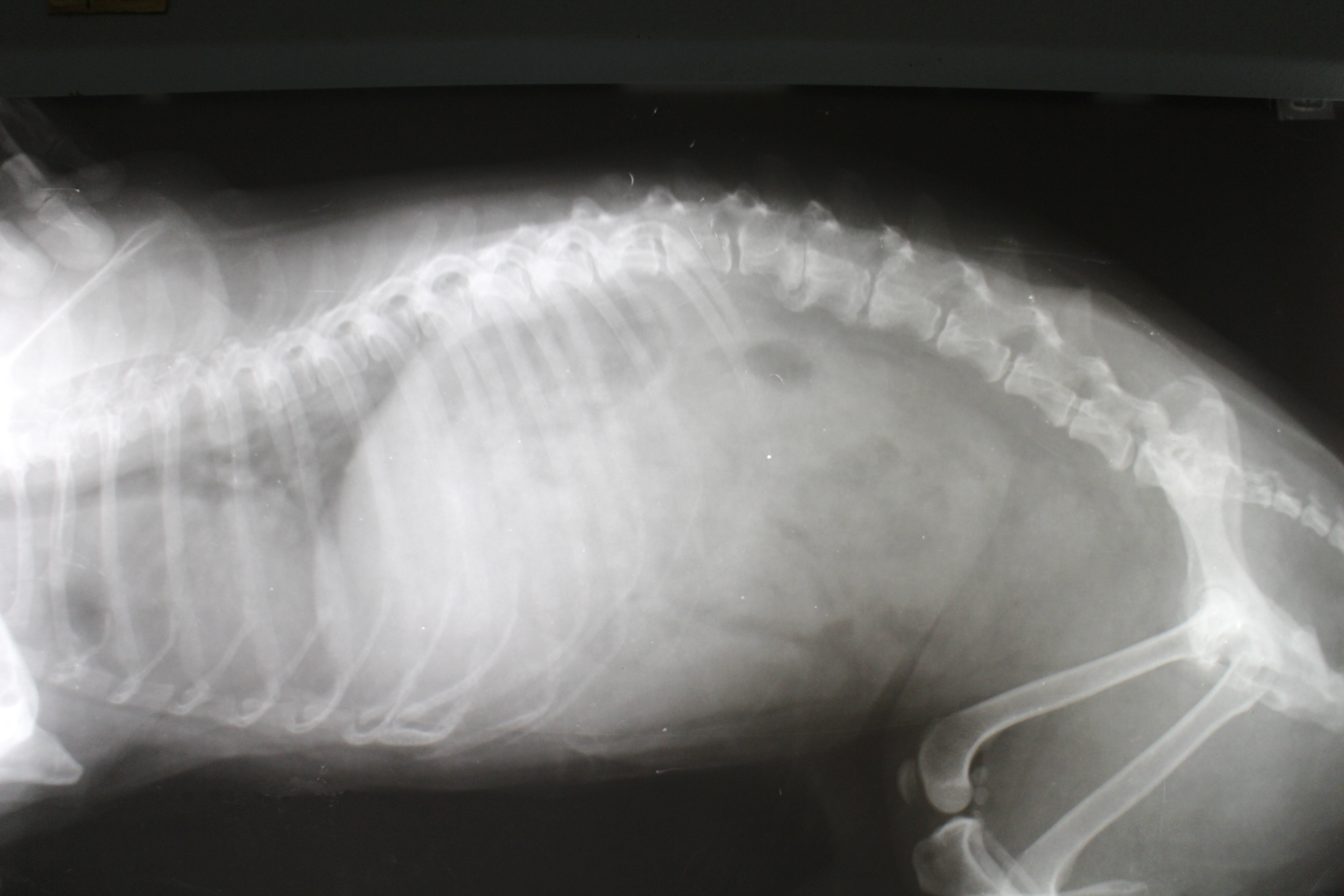
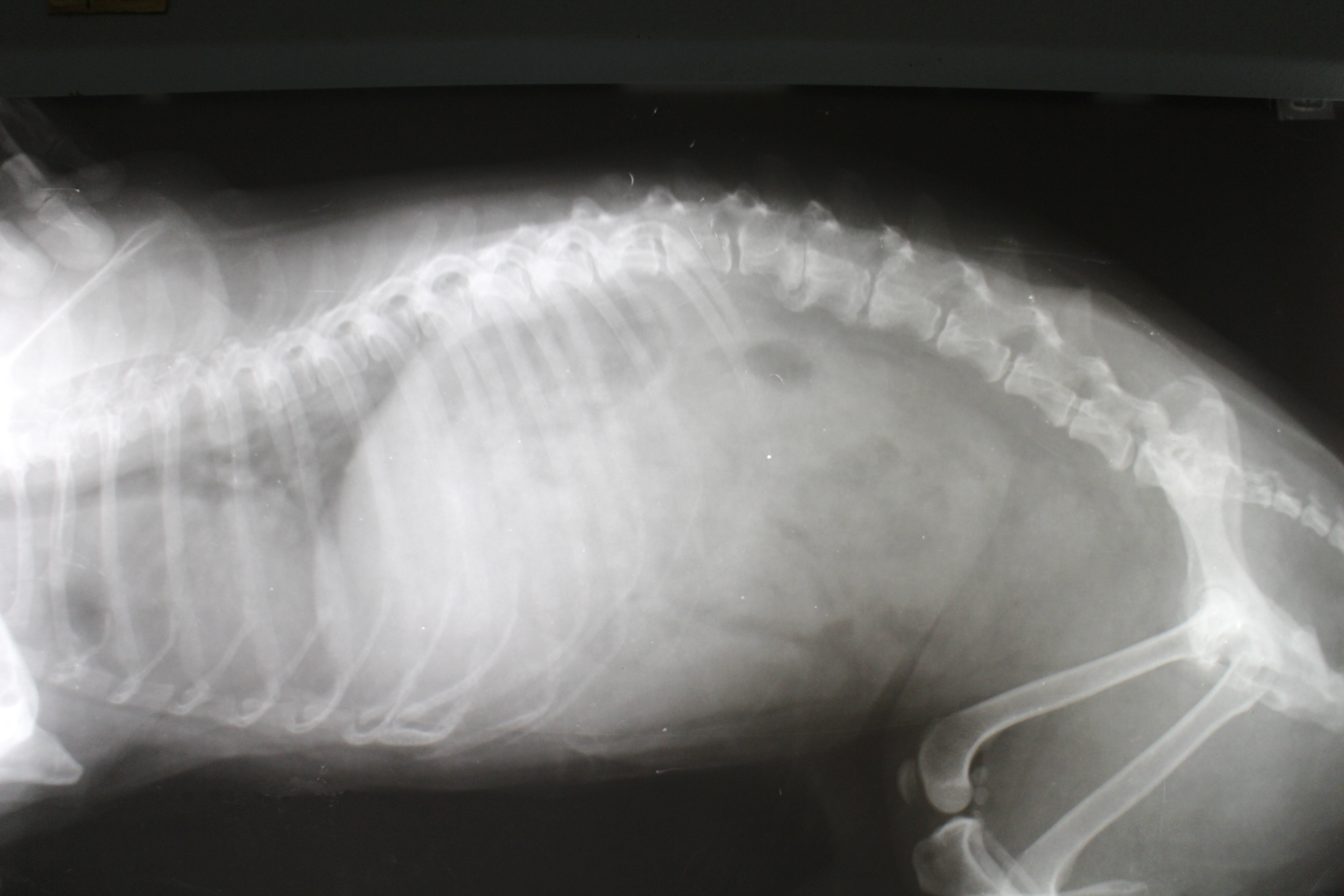
Veterinarians Keep Close Watch on Potentially Deadly Canine Disease – New Website Profiles the Latest Info on Recent Outbreak of Leptospirosis – From Boston and Buffalo, to Chicago, Denver, Houston and San Diego, veterinarians across the country are keeping a...

by Ken DeRouchie | May 29, 2007 | Articles, Featured Optometry, Issue 03, Newsletter, Optometry, Practice Areas
SURVEY OF OPTOMETRISTS SHOWS FINANCES AND STAFF AS MAJOR PROBLEMS AFFECTING GROWTH In the second in a series of articles addressing surveys The Practice Solution Magazine has conducted on the optometry, veterinary and dentistry professions, we are releasing the...
by Ken DeRouchie | May 29, 2007 | Articles, Featured Optometry, Issue 04, Newsletter, Optometry, Practice Areas
WASHINGTON /PRNewswire-FirstCall/ — Halozyme Therapeutics, Inc. a development stage biopharmaceutical company focused on the development and commercialization of recombinant human enzymes, announced that results from new preclinical studies with Halozyme’s recombinant...